Thank you for downloading!
Subscribe to our newsletter to receive email updates about our work, get connected and support Australians impacted by eczema. You can unsubscribe at any time.
Subscribe NowFacial eczema is a skin condition that can vary in severity, from occasional flare-ups to more chronic or recurring episodes. It can be linked to atopic eczema, contact dermatitis, or seborrhoeic dermatitis. The sensitive nature of facial skin makes the discomfort from eczema more noticeable and distressing. It can affect both children and adults, often appearing on areas like the cheeks, eyelids, and around the mouth.
In babies, facial eczema commonly affects the cheeks and neck folds, while older children and adults may experience more widespread eczema, including on the eyelids. Regardless of age, the visibility of facial eczema can impact quality of life, making effective treatment and management crucial.
Visit our Online Toolkit to find the best way to care for your facial eczema.
Go To Toolkit
facial eczema
Facial eczema may develop as a result of various factors, including:
Seborrhoeic dermatitis, another form of eczema, can lead to greasy scales around the ears, eyelids, or eyebrows and is commonly associated with dandruff.

Facial Eczema
The symptoms of facial eczema can vary depending on the type and severity, but the most common signs include:
Redness and Inflammation: Skin on the face may appear red and swollen.
Dry, Flaky Skin: The skin may peel or crack, causing discomfort and sensitivity.
Itchiness: Persistent itching is common, which can lead to scratching and further irritation.
Pain or Burning Sensation: In more severe cases, eczema may cause a burning feeling or pain, especially when exposed to certain irritants.
Thickened or Rough Skin: With chronic eczema, the skin may thicken or become leathery.
Blisters: In rare cases, blisters may form, which can break open and become infected.

facial eczema
A big part of managing facial eczema is avoiding irritants and controlling inflammation. Some common irritants to be aware of include:
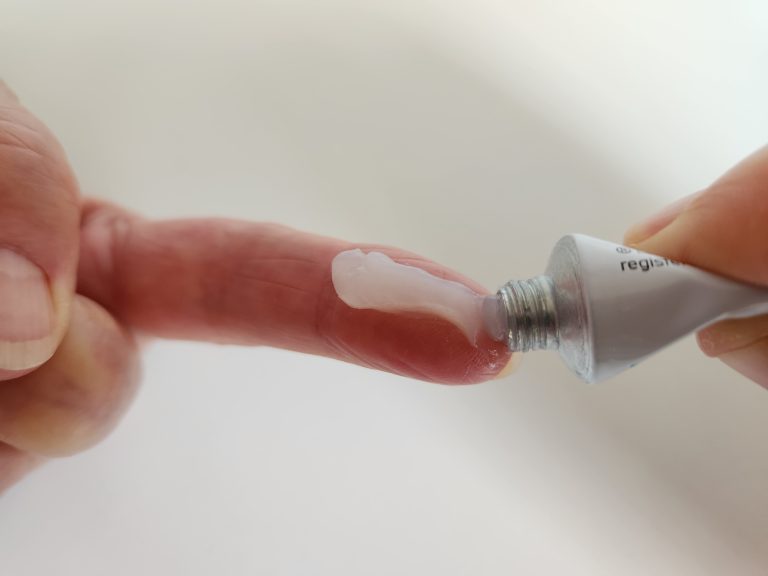
For those with atopic eczema, it’s important to apply an emollient at least twice a day to help protect and hydrate the skin.

facial eczema management
facial eczema
Your doctor may prescribe a topical corticosteroid or a topical calcineurin inhibitor to treat flare ups.
Effective treatment for facial eczema requires a multi-faceted approach that targets both symptom relief and long-term prevention.
Topical corticosteroids for eczema come in a cream, ointment or lotion (for the scalp), and you may be prescribed a mild or moderate strength for your facial eczema to be used in short treatment bursts as directed by your doctor. Potent steroids are rarely prescribed for the face and never used around the eyes, however, a potent corticosteroid may be appropriate for the scalp or the forehead, where the skin is thicker. If you are prescribed a potent steroid, be sure to use it under the supervision of a dermatologist.
You may be prescribed non-corticosteroid topical therapy (pimecrolimus, tacrolimus or crisaborole) for treatment of your facial flares. For seborrhoeic dermatitis, an anti-yeast cream may be used along with a mild corticosteroid.
facial eczema
For more severe cases of facial eczema, there are emerging treatments offering relief. While eczema can be overwhelming, medical research continues to provide new solutions. Speak with your dermatologist about the latest treatment options and potential therapies that may suit your condition.

Seborrhoeic Dermatitis
Facial Eczema
In cases where seborrhoeic dermatitis is contributing to facial eczema, you may need a combination of treatments:
Facial Eczema
Establishing a good skincare routine is essential for managing facial eczema. Follow these steps to help maintain your skin’s health:

The triggers of eczema are often different for each individual. It can be extremely frustrating as you try to work out the cause of each flare up.
Avoiding triggers and controlling flare ups/inflammation are ways in which you can manage your condition. But there is rarely just one trigger that will be responsible.
e.g. coarse, scratchy wool, synthetic materials like polyester, tags, on clothing
such as soaps and detergents.
Although there may be a link between food allergies and eczema, food is rarely the main eczema trigger (seek doctors/allergist/immunologist advice before eliminating foods)
can both seriously aggravate eczema. Herpes simplex (cold sores) may become widespread and require hospitalisation.
associated with sweating
which cause allergic contact dermatitis such as perfume, preservatives in skincare products, metals such as nickel and many other.
if there is an allergy to household dust mite.
Facial eczema can be influenced by genetics (family history of eczema) and external factors such as exposure to irritants or allergens. It can also be triggered by stress or conditions like seborrhoeic dermatitis, which often manifests with greasy scales around the ears, eyelids, or eyebrows. Identifying specific triggers can be challenging, but avoiding known irritants is key.
Visit the Eczema Resource Library to learn more.
Use our Eczema Care Online Toolkit to find out the best way to care for your eczema or your child's eczema.
Subscribe to our newsletter to receive email updates about our work, get connected and support Australians impacted by eczema. You can unsubscribe at any time.
Subscribe Now